Applying the Social-Ecological Model to the optimal recovery path post Traumatic Brain Injury
- Tanya Zeron
- Oct 23, 2023
- 5 min read
Updated: Nov 6, 2023
The journey through rehabilitation from a Traumatic Brain Injury (TBI) is diverse, each case following a unique trajectory. There is an optimal path to recovery that reflects what is attainable for the individual under the best conditions. However, the path can vary for individuals, Social Determinants of Health ( SDoH) can either provide opportunity or hamper the road to the optimal path of rehab. The Institute of Medicine defines the Social Ecological Model (SEM) as a model of health that emphasizes the linkages and relationships among multiple factors affecting health. (2003) The SEM encompasses various levels starting with the individual, interpersonal, community, and social political. We will apply each level of the SEM to the context of TBI rehabilitation.

Individual factors Individual factors comprise of age, race, ethnicity, gender and behavior. When and individual sustains a TBI, particularly in the frontal love, it often results in challenges related to memory, emotional regulation, impulse control, problem-solving, and impulsivity. Deficits in insight, and impulsivity can present as uncontrollable adverse behaviors, these behaviors can have profound consequences for the individual, potentially hindering their ability to return to their previous level of functioning. As Shames pointed out, if the post injury status prohibits the individual from returning to the workforce, this can have profound consequences to the individual and family, both economic and psychosocial. (2019)
In British Columbia an individual without private insurance can seek financial assistance through the Ministry of Social Development and Poverty Reduction (MSDPR). Monthly this amounts to $1483.50 (Government of BC, 2023) The cost of living, compounded with the housing crisis in British Columbia poses a significant challenge, that can further steer the recovery journey farther from the optimal path. It is important to consider if the individual age, race, and behaviors provided them the opportunity to purchase private insurance. Such insurance can provide them with their previous wage and long-term disability benefits, thereby steering their recovery journey closer to the optimal path.
Interpersonal and Institutional relationships encompass the social support the individual has and family characteristics. Research conducted by Juliet Haarbauer-Krupa has highlighted the impact of social cognition in adult civilians. Haarbauer-Krupa found individuals effected by TBI showed a significant reduction of social inference-interpreting verbal and non-verbal social cues. (2002) The implications of impaired social inference go beyond the individual, potentially affecting their capacity to maintain employment or stable housing, as previously highlighted. Individuals residing in subsidized housing need to interact with a diverse group of people, deficits in social inference and uncontrollable adverse behaviors can lead to poor social outcomes and social isolation. In the worst-case scenario if behaviors are unmanageable the individual can be at risk of homelessness.
Family and Interpersonal relationships can positively steer the individual towards the optimal path of recovery. Research by Donald Berwick and colleagues highlighted that family/friend involvement during inpatient rehabilitation can have a lasting positive impact on an individual’s community participation and cognitive functioning for up to nine months post discharge. (2022) The acute medical model focuses on functional deficits for the purpose of activities of daily living but does not focus on the individual in their social setting. "Families and caregivers of people with TBI continue to report significant burdens and unmet needs." (Donald Berwick, et al., 2022) This goes to show the relationship the individuals have with their family and the family's ability to navigate the healthcare system can steer them towards or away from the optimal path of recovery.
Community Environment- encompass many settings such as workplaces, schools, service systems, transportation networks, and geographic location, can have a vital role in the rehabilitation journey. Research done by Berwick has highlighted the negative outcomes of sustaining TBI in relation to residence in rural or high poverty areas. (2022) In a rural setting there are geographical barriers that hinder quick access to specialized care available at trauma centres. Rural communities have limited access to public resources and rely more on volunteer emergency responders. “Service providers in urban settings or specialized trauma care where healthcare providers have more frequent opportunities to practice and maintain their specialized skill set.” (Brown, 2019)
Brown evaluated TBI mortality rates across urban and rural regions in the United States, revealing a significant disparity, with the TBI fatality rate being 13 deaths per 100,000 individuals higher in the most rural areas compared to the most urban areas. (Brown,2019) The disparities in the individual’s community and accessibility to healthcare resources in rural areas can influence the direction of an individual recovery journey, potentially steering them away from the optimal path of rehabilitation.
Social, economic and political influences can come together to reduce health inequalities and an individual’s recovery trajectory. Consideration of the Social Determinants of Health (SDoH) is essential, as research highlights the disproportionate prevalence of TBI among individuals contending with adverse SDoH, including unemployment, lower levels of education, and low socio-economic status (Chan.2022)
The Centre for Disease Control and Prevention (CDC) has started initiatives aimed at advancing health equity for individuals affected by TBI. These initiatives include different components, including the collaborative development of programs for service members and veterans living with TBI, the promotion of the CDC's Roadway to Safer Tribal Communities Toolkit, which is designed to prevent motor vehicle crashes responsible for a significant number of TBI-related deaths among American Indian and Alaska Native populations, and the establishment of telehealth programs to train rural primary care providers and school professionals, enhancing TBI care for children (CDC, 2023).
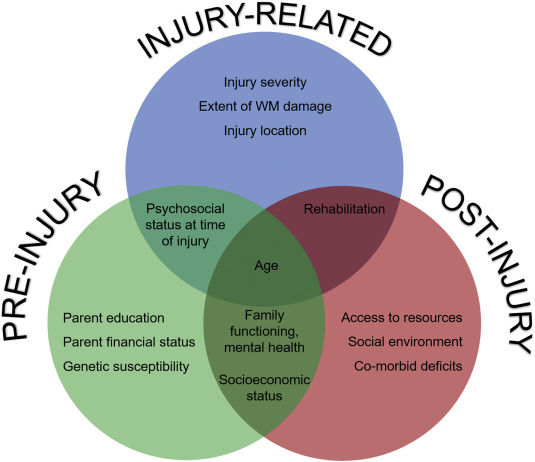
As demonstrated above, using the framework from Bronfenbenner's Social-Ecological model, we can see that injury and recovery are influenced by an interplay between physical and medical, psychological and behavioural, and social and economic factors. All of these factors can interact to compound or exacerbate inequities in outcomes, and access to care across different populations of TBI patients (Brown, 2019) Further research needs to be completed to fully understand the effects of TBI on the healthcare system so we can develop policy to increase health equality.
Below is a model of the causation of the social determinants of health that I found helpful in broadening my understanding of how SDoh contributes to health inequalities.

Works Cited
Akram Zamani, Richelle Mychasiuk, Bridgette D. Semple,
Determinants of social behavior deficits and recovery after pediatric traumatic brain injury, Experimental Neurology, Volume 314,2019,Pages 34-45,
ISSN 0014-4886,
Brown, J. B. (2019). Geographical Disparity and Traumatic Brain Injury in America: Rural Areas Suffer Poorer Outcomes. Journal of neurosciences in rural practice, 10(1), 10-15.
Centers for Disease Control and Prevention. (2023). Retrieved from Traumatic Brain Injury & Concussion: https://www.cdc.gov/traumaticbraininjury/index.html
Chan, V. (. (2022). Social determinants of health associated with psychological distress stratified by lifetime traumatic brain injury status and sex: Cross-sectional evidence from a population sample of adults in Ontario, Canada. PLoS ONE, Vol. 17 Issue 8, p1-15. 15p.
Donald Berwick, K. B., Care, C. o., Policy, B. o., Services, B. o., Division, H. a., & Academies, N. (2022). Traumatic Brain Injury: A Roadmap for Accelerating Progress (2022). Washington, DC: The National Academies Press.
Jeffrey Shames 1, I. T. (n.d.). Return to work following traumatic brain injury: trends and challenges. Disability and rehabilitation,, 29(17), 1387–1395.
Jonathan E. Fielding, M. M. (2013). A Perspective on the Development of the Healthy People 2020 Framework for Improving U.S. Population Health. Public Health Reviews, 35(1), 1–24. .
Juliet Haarbauer-Krupa, M. J. (2022). Epidemiology of Chronic Effects of Traumatic Brain Injury. Journal of Neurotrauma , 38:23, 3235-3247 .



Comments